
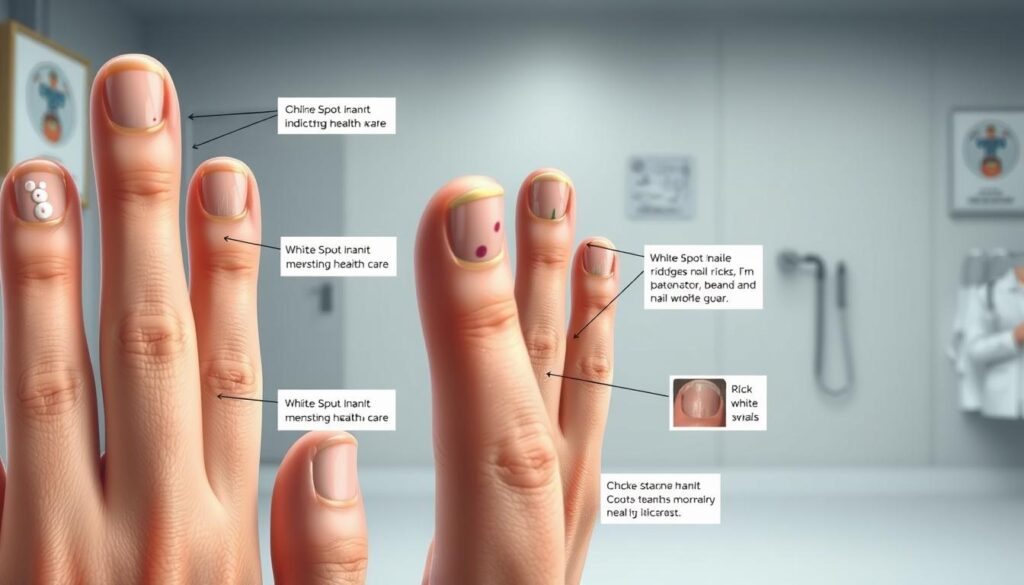
Have you ever glanced at your hands and noticed unexpected marks that make you question your health? Those pale specks or streaks might seem like harmless quirks, but they could hold clues about your body’s inner workings. Known medically as leukonychia, these markings often spark curiosity—and sometimes concern—about their origins.
According to dermatologist Dr. Karan Lal, these discolorations typically stem from minor injuries to the nail bed. Think: accidentally bumping your finger or aggressive manicures. While they’re most common in kids (hello, playground adventures!), adults aren’t immune. The good news? Most fade as your nail grows out naturally.
But here’s the twist—occasionally, these specks signal more than just a bump or scrape. Nutritional gaps, allergies, or even certain medications might leave similar traces. Learning to spot the differences helps you decide when to shrug it off or consult a professional.
Key Takeaways
- Most discolorations result from minor injuries and resolve on their own
- The medical term for this condition is leukonychia
- Persistent or widespread markings may require medical evaluation
- Proper nail care reduces the risk of future damage
- Nutritional factors can occasionally play a role
Ready to decode what your nails reveal? Let’s explore how to distinguish everyday causes from rare red flags—and keep your fingertips looking their best.
Understanding Leukonychia

Your fingernails act as tiny health dashboards, revealing patterns worth decoding. When those pale marks appear, dermatologists call it leukonychia—from the Greek words for “white” and “nail.” Dr. Brendan Camp clarifies:
“This term describes any abnormal whitish discoloration in the keratin layers.”
Definition and Overview
True leukonychia starts at the nail matrix—the growth factory beneath your cuticle. These specks travel outward as your nail grows and stay visible when pressed. Unlike temporary marks from bumps, they’re baked into the nail plate itself.
Types to Recognize
Apparent leukonychia plays hide-and-seek. Press your fingertip, and these bed-level discolorations vanish briefly. They often hint at circulation issues or underlying skin conditions.
Fungal infections cause pseudoleukonychia, creating chalky flakes on the surface. Unlike other types, these respond to antifungal treatments rather than waiting for nail growth.
Three specialized forms complete the picture:
- Partial: Confetti-like dots from minor injuries
- Longitudinal: Vertical streaks signaling matrix damage
- Transverse: Horizontal bands linked to systemic stressors
Knowing these distinctions helps you track whether those marks need patience or professional insight. Spot the pattern, then decide your next move.
Common Causes of White Spots on Nails

Those pale markings on your fingertips often start with everyday mishaps you might not even notice. Let’s break down the usual suspects—from accidental bumps to beauty routines gone wrong.
When Bumps Leave Clues
Minor injuries account for most cases. Stubbing a toe or slamming a finger in a drawer disrupts the nail matrix—the growth hub under your cuticle. These marks typically show up weeks later as your nail grows out.
Habits matter too. Frequent nail-biting or wearing tight shoes creates repeated stress. Even vigorous manicures with metal tools can dent the delicate surface layers.
Beauty Treatments Backfire
That fresh set of acrylics might come with hidden costs. Harsh chemicals in gel polishes or adhesives can trigger allergic responses. Look for these red flags after salon visits:
- Sudden chalky patches under polish
- Peeling or brittleness around edges
- Itching or redness near cuticles
Acetone-based removers strip natural oils, leaving nails parched and prone to damage. Switching to gentler formulas often helps prevent future issues.
Spotting patterns helps you take action. Did those marks appear after gardening without gloves? Or maybe following a new nail product trial? Your timeline holds answers.
Fungal Infections Behind White Spots on Nails

While many associate nail issues with yellowing, some stealthy invaders leave a different calling card. Dr. Brendan Camp notes:
“Fungal infections can create pale discolorations that mimic harmless marks, requiring closer inspection.”
These cases account for 14% of nail disorders, often targeting vulnerable groups like older adults or those with diabetes.
Identifying Fungal Symptoms
Superficial white onychomycosis plays tricks with its chalky surface flakes. Unlike injury-related marks, these patches don’t fade when pressed. Watch for:
- Crumbling texture near nail edges
- Musty odor from affected areas
- Spread to adjacent nails over weeks
Public pools and gym showers become risk zones—fungi thrive in warm, damp surfaces. Previous injuries or foot deformities create entry points, letting spores take hold.
Prevention and Early Intervention
Keep feet dry and wear breathable shoes after workouts. Avoid sharing nail tools, and disinfect clippers regularly. Suspect an infection? Don’t reach for drugstore creams first.
Lab tests confirm diagnoses through nail scrapings. Prescription antifungals work better when started early, preventing spread to household members. Remember: these infections dig deep, so patience with treatment timelines matters.
Impact of Medications on Your Nails

Your prescription might be doing more than you realize—even leaving traces on your fingertips. While most people focus on internal effects, certain drugs can alter nail growth patterns. Dermatologist Dr. Karan Lal notes:
“Medications ranging from cancer treatments to common antibiotics often create visible changes patients don’t expect.”
Chemotherapy and Long-Term Antibiotics
Chemotherapy agents frequently cause markings because they target fast-growing cells. This includes nail matrix cells responsible for creating keratin layers. These changes typically appear weeks after treatment starts as nails grow out.
Long-term antibiotic use—especially sulfa drugs—can disrupt your nail’s microbiome. This imbalance sometimes leads to surface irregularities or temporary discoloration. Other culprits include:
- Blood pressure medications affecting nutrient absorption
- Retinoids altering skin and nail cell turnover
- Anti-seizure drugs interfering with mineral metabolism
Always notify your doctor about new nail changes after starting treatments. Many medication-related marks fade naturally once your body adjusts or the prescription ends. Tracking timelines helps identify connections without interrupting vital therapies.
Underlying Medical Conditions to Consider
Your fingertips might reveal more than you realize. While most markings fade harmlessly, some patterns demand attention. Dermatologist Dr. Karan Lal emphasizes:
“Specific discoloration patterns can act as early warnings for systemic health issues needing professional care.”
Liver, Kidney, and Heart Indicators
Half-and-half nails show a clear horizontal divide. The lower portion appears milky, while the upper remains pink. This pattern often signals kidney disease. Dr. Lal notes it appears in 40% of dialysis patients.
Muehrcke’s lines—paired white bands—often indicate low albumin levels. This protein deficiency links to liver issues or malnutrition. Watch for these across multiple nails simultaneously.
| Condition | Nail Sign | Associated Symptoms |
|---|---|---|
| Kidney Disease | Half-and-half nails | Swelling, fatigue, urination changes |
| Liver Issues | Muehrcke’s lines | Jaundice, abdominal swelling |
| Heart Failure | Pale nail beds | Shortness of breath, leg swelling |
Autoimmune disorders like lupus may create red-and-white streaks alongside joint pain. Blood disorders such as sickle cell anemia often cause spoon-shaped nails with unusual markings.
When multiple nails show changes paired with symptoms like unexplained fatigue or swelling, schedule a checkup. Early detection helps manage these conditions effectively.
Nail Damage from Daily Habits and Lifestyle
Your daily routine might leave marks you never expected—right at your fingertips. Common practices like tapping surfaces or frequent salon visits often impact nail health more than you realize. Let’s explore how small choices add up over time.
Hidden Costs of Beauty Routines
Dr. Brendan Camp warns: “Manicures and pedicures often use tools that weaken the nail plate.” Harsh chemicals in polishes and removers strip natural oils, creating dry layers prone to damage. At professional nail services, technicians sometimes over-file surfaces or apply excessive pressure during cuticle work.
Nail-biting introduces double trouble—trauma to the growth matrix and bacterial exposure. These habits create lasting marks that take months to grow out. Even seemingly harmless tics like tapping your desk chip away at protective layers.
Dr. Karan Lal advises: “Swap acetone removers for gentler formulas and let nails breathe between treatments.” Simple changes help maintain strength while reducing risks. Your hands work hard—give them care that lasts beyond the polish.
