
Worried about thinning or unusual shedding? It’s normal to lose about 50 to 100 strands each day. But illness, hormones, stress, aging, or genetics can push that number higher and slow new growth.
Good options range from over-the-counter minoxidil and prescription finasteride to office procedures like grafting, low-level laser therapy, PRP, and scalp micropigmentation. Some thinning after childbirth, surgery, or heavy stress often improves as the body heals.
This guide walks you through what’s normal, why causes differ, and which routes match your goals. You’ll learn when products make sense, when to see a provider, and how gentle care and lifestyle choices support a fuller head.
Expect clear timelines and realistic outcomes. We’ll also explain how clinicians assess causes so people get targeted plans instead of guessing.
Key Takeaways
- Normal daily shedding occurs, but persistent increases need review.
- Options include OTCs, prescriptions, and in-clinic procedures like PRP and grafting.
- Causes vary; a proper exam and history guide the best path.
- Lifestyle and gentle care help recovery after stress or illness.
- Combining approaches can improve growth and coverage.
- Realistic timelines help set expectations for visible results.
What this Ultimate Guide Covers and Who It’s For
This guide maps clear steps you can take, from everyday care to clinical options, so you know what to try and when to seek help.
Many effective options exist that can slow hair loss and support new growth. A healthcare provider or dermatologist can help you choose choices that match your health and goals.
It’s normal to shed about 50–100 strands a day. Shedding above 100 per day, a receding hairline, or sudden patchy loss are reasons to seek guidance.
- Who this is for: people noticing persistent thinning, comparing drugstore items to prescriptions, or planning long-term scalp health.
- What’s covered: causes and types hair loss, diagnosis steps, OTC and prescription treatment paths, in-office procedures, natural support, and safety.
- Practical tools: timelines, maintenance advice by age and sex, checklists to start, stack, or switch approaches, and questions to ask your clinician.
By the end, you’ll have a clear action plan and next-step questions to bring to your provider.
| Audience | Common Issues | Recommended Path | Expected Timeframe |
|---|---|---|---|
| Early thinning | Diffuse shedding, mild thinning | Daily home care + OTC or prescription review | 3–6 months to assess |
| Sudden patchy loss | Alopecia areata or medical causes | See dermatologist for diagnosis and targeted therapies | Weeks to months, varies by condition |
| Long-term pattern | Receding hairline, patterned thinning | Medications, procedures, or combined plans | 6–12 months to see meaningful change |
Understanding Hair Loss and Thinning Hair: Causes, Types, and What’s Normal

Knowing when everyday shedding becomes a medical concern helps you act early and wisely.
Normal shedding is about 50–100 strands a day. If you see steady clumps, a widening part, or persistent thinning, that suggests excessive loss and needs attention.
How the growth cycle explains shedding
The growth cycle moves follicles through growth, rest, and shedding phases. Illness, hormones, or stress can push more follicles into rest, causing greater loss without equal regrowth.
Common causes and reversible triggers
Genetics and hormonal shifts are major drivers, but age, medical conditions, certain meds, and lifestyle choices matter too. Tight styles, frequent chemicals, heat, and nutrient shortfalls (iron, vitamin D, zinc) worsen thinning.
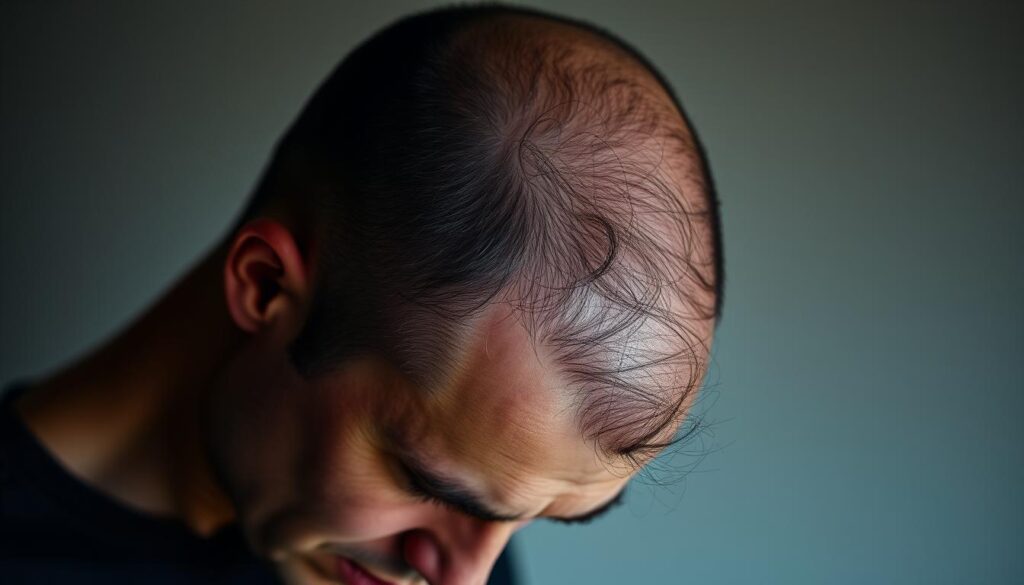
Thinning versus pattern baldness
Thinning hair often looks like diffuse density loss across the scalp. Pattern baldness shows predictable recession at the hairline or crown and changes the shape of the head over time.
- Postpartum, surgery, or severe stress can cause temporary shedding that often improves as the body recovers.
- If loss is patchy, rapid, or comes with scalp itching or scaling, seek medical evaluation.
Understanding the main drivers—genetic pattern, hormonal change, inflammatory conditions, or external stressors—helps match the right approach and decide when to escalate care.
Getting a Diagnosis: Identifying the Underlying Cause Before Treatment

Diagnosis begins with careful questions and a hands‑on exam to avoid guesswork.
What clinicians evaluate
- Your history: onset, pattern, recent illness, medications, pregnancy, diet, and family background to narrow the likely type hair loss.
- Physical exam: a close look at the scalp and skin to spot scaling, redness, scarring, or inflammation that points to specific conditions.
- Blood work: tests may include iron studies, folate, vitamin D, and thyroid markers to detect medical conditions that drive shedding.
When to seek care
If you notice more than about 100 hairs a day, a rapidly receding hairline, or sudden patchy loss, schedule an evaluation promptly.
Why diagnosis matters
Finding the cause first reduces trial‑and‑error and lets providers target therapies safely. You’ll discuss goals—thickening, regrowth, or coverage—and get a realistic time plan.
| Evaluation Step | What to Expect | Why it Matters |
|---|---|---|
| History | Questions on onset, meds, diet, and family | Narrows the likely type hair loss and guides tests |
| Exam | Scalp and skin inspection; photos taken | Identifies dermatologic causes and tracks progress |
| Blood tests | Iron, vitamin D, thyroid, and related markers | Finds correctable medical conditions that can stop shedding |
Evidence-Backed hair treatment for hair loss: OTC and Prescription Options

Simple, evidence-backed products and select prescriptions form the backbone of most medical regrowth plans.
Over-the-counter choices include topical minoxidil (FDA-approved for pattern baldness) and anti-thinning shampoos. Apply minoxidil daily and allow up to 16 weeks to judge effects. Many store products list biotin, zinc, collagen, azelaic acid, or tea tree oil, but evidence varies.
Prescription medications and who they suit
Finasteride is an approved prescription for men with patterned decline; it’s usually avoided in premenopausal women. Spironolactone can help females with hormonally driven loss due to anti-androgen action.
Corticosteroids when autoimmune causes exist
Topical steroids or scalp injections every 4–6 weeks reduce inflammation in alopecia areata and can encourage regrowth under dermatology care.
Daily use, timelines, and monitoring
- Commit to daily application or dosing and use photos to track subtle change.
- Combine over-the-counter products with prescription medication when recommended.
- Watch for side effects like scalp irritation or systemic changes and report them early.
| Option | Who it’s for | When to expect changes |
|---|---|---|
| Minoxidil (topical) | Patterned thinning, both sexes | Up to 16 weeks; ongoing use needed |
| Finasteride (prescription) | Men with pattern baldness | 3–6 months to assess response |
| Spironolactone (prescription) | Women with hormonal thinning | 3–6 months; monitor labs |
| Corticosteroids (topical/injection) | Alopecia areata or inflammatory types | Weeks to months with repeat injections |
Procedures and Devices: From Hair Transplants to Laser Therapy

Modern office procedures and devices can add density or camouflage visible thinning without months of trial-and-error.
Grafting (transplant) and scalp reduction
Grafting moves your own follicles from a donor zone to pattern baldness areas. It is an outpatient process done under local anesthetic. Expect an aftercare plan to protect grafts and nearby skin.
Scalp reduction removes non‑growing skin so nearby scalp stretches to cover gaps. It helps the top and back of the head but rarely improves the frontal hairline.
PRP and laser options
PRP draws a small amount of blood, spins it in a centrifuge, and injects concentrated platelets into the scalp. Downtime is minimal and results appear over months.
Low-level laser therapy (LLLT) uses medical-grade light to stimulate follicles. It works in clinics or via at-home devices, and multiple sessions are needed to see effects.
Scalp micropigmentation and combined plans
Micropigmentation is a specialized tattoo that masks thinning or bald spots without surgery. It suits those seeking cosmetic density or a close-cropped look.
“Match the method to your pattern, donor limits, and goals, and plan maintenance with your provider.”
- Expect local anesthesia and clear aftercare after grafting.
- Combine procedures with minoxidil or medical plans to protect existing strands.
- Discuss cost, recovery time, and skin sensitivity before deciding.
| Procedure | Best area | Downtime | Typical timeline |
|---|---|---|---|
| Grafting | Crown, mid‑scalp | Days to a week | 6–12 months |
| Scalp reduction | Top/back of head | Weeks | Months |
| PRP | Diffuse thinning | Minimal | 3–6 months |
| LLLT | Diffuse areas | None to minimal | Months of sessions |
| Micropigmentation | Any visible thinning | 1–2 days | Immediate cosmetic effect |
Natural Ways to Support Hair Growth Without Formal Treatment
Return to balance often helps follicles recover after a major trigger. A pause in pregnancy‑related shifts, surgery, or severe stress can allow natural growth to resume over weeks to months.
When regrowth is likely
Many people note steady improvement after the body heals from illness, major weight loss, or intense stress. Give the scalp time while you track shedding each day.
Lifestyle upgrades that help
- Eat a balanced plate with protein, iron, folate, and zinc to support follicle health.
- Reduce stress with walks, short meditations, and better sleep—small daily habits add up.
- Quit smoking and limit alcohol; these moves improve scalp circulation and overall health.
Gentle care to minimize breakage
Choose milder products, avoid tight styles, and lower heat use. Use a heat protectant when needed and favor looser looks to protect the hairline.
- Track changes and talk to a clinician if thinning persists beyond a few months.
Safety, Side Effects, and Setting Realistic Expectations
Before starting any plan, know the common risks and what to watch for during early weeks.
Medications and procedures can help, but they carry real side effects. Minoxidil may cause scalp irritation and must be used continuously to keep gains; visible effects can take up to 16 weeks. Finasteride has specific risks and is not recommended in people who may become pregnant. Spironolactone can cause dizziness or headaches and needs monitoring.
Procedures vary in downtime and risk. Discuss how your skin and scalp might react, what aftercare looks like, and when to adjust the plan if healing stalls.
Essential oils have limited human evidence and can cause allergic reactions. Always dilute, patch test, and stop at the first sign of irritation. Supplements help only when labs show a deficiency; excess intake can harm or interact with existing medications.
- Expect stages: less shedding, thicker feel, then visible density over months.
- Many approaches require ongoing maintenance; stopping suddenly can reverse gains.
- If you have other medical conditions, review interactions before adding products.
| Risk area | Common side effects | When to contact a clinician |
|---|---|---|
| Topical medications | Scalp irritation, itching | Persistent redness or pain |
| Oral medications | Dizziness, hormonal effects | New systemic symptoms |
| Procedures/devices | Swelling, temporary sensitivity | Infection or delayed healing |
Conclusion
, Your next step is a clear, simple plan that fits your goals and timeline.
Many types of thinning are treatable when you match the right approach to the diagnosis. Start with a clinician visit to identify the pattern and rule out medical causes.
Combine daily care, lifestyle steps, and targeted treatment when needed to protect existing follicles and encourage growth. Expect changes in stages over months and plan maintenance to keep gains.
If you have advanced baldness or a changing part, surgical and cosmetic options can restore a natural look. When sudden patches or persistent excess shedding appear, seek prompt evaluation to preserve more coverage.
